Introduction
Immune thrombocytopenia (ITP) is an autoimmune disease characterized by accelerated platelet destruction with impaired platelet production leading to a platelet count decreased +/- bleeding manifestations, mostly caused by antiplatelet autoantibodies. The role of monocytes in ITP pathophysiology is not clearly established. Circulating monocyte subpopulations were identified phenotypically by flow cytometry and defined according to the surface expression of CD14 and of CD16 into classical (cMo), intermediate (iMo) and nonclassical (ncMo) monocytes. A new subpopulation, defined by the expression of the slan marker, has recently been described and represents a fraction of ncMo (ncMo slan +).
Objectives
The 1 st objective of the study was to analyze the partitioning of peripheral blood monocyte subsets by flow cytometry in ITP patients compared to a group of healthy blood donors (HD). Our second objective was to further characterize different phenotypic profiles of monocytes among ITP patients based on baseline characteristics, severity and treatment(s).
Methods
From April 2019 to January 2023, peripheral blood samples from ITP patients and HD were collected on EDTA and stained with the following antibodies: anti-CD45, CD2, CD56, CD24, CD14, CD16 and anti-slan. Acquisition analysis was performed either with a Navios or a DxFLEX cytometer. All files were analyzed with the previously described exclusion strategy of non-monocytes populations, using Kaluza™ analysis software, to characterize cMo, iMo, ncMo and ncMo slan + subsets. ITP patients were included regardless of their ITP status and/or phase of the disease.
Results
In total, 56 peripheral blood samples from 46 ITP patients and from 19 HD were analyzed. ITP patients had a median age of 50.5 years [19-91], 54.3% were females, whereas the median age of HD was 36 years [21-65] with 42.1% of females. ITP was defined as primary in 82.6% of the cases with a median disease duration of 3 years (<3 months or newly-diagnosed in 26.8% and >12 months or chronic ITP in 60.7%). Nine patients had undergone splenectomy (19.6%) at time of analysis. The platelet count was <50 x 10 9/L in 60.7% of ITP patients and absolute monocyte count ≥ 1 x 10 9/L was found in 21.4%. Regarding ITP treatment, 14 patients (25%) were receiving glucocorticoids (GC) at time of analysis whereas 9 (16.1%) had been exposed to GC within the previous month. Eleven patients (19.6%) had received intravenous immunoglobulin within a month prior to the analysis, 20 (35.7%) were on thrombopoietin receptor agonists, 9 (16.1%) had received rituximab in the previous year, 4 (7.1%) received another immunosuppressive therapy and 6 (10.7%) received another treatment. Eighteen patients (32.1%) were considered as “treatment-free” as they had not received any treatment for their ITP in the previous month or rituximab in the previous year. The latter group of “untreated” patients displayed a significant increase of the iMo relative fraction when compared to HD (4.92% vs 3.18%, p=0.018). There was no significant difference between the two groups regarding other monocytic subpopulations, including cMo, ncMo, ncMo slan+, the absolute and relative counts of monocytes.
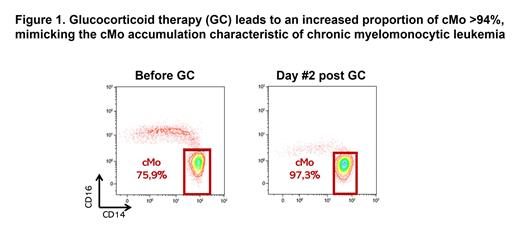
As for the treatment effect, the ongoing intake of GC therapy did not have a significant impact on monocytosis but was strongly associated with an increased proportion of cMo (94.2% vs 85.0%, p < 0.0001; Figure 1) and a decreased proportion of ncMo (2.31% vs 9.85%, p<0.0001) and ncMo slan+ (3.12% vs 7.46%, p<0.0001), mimicking the cMo accumulation characteristic of chronic myelomonocytic leukemia. Splenectomy and other treatments did not significantly interfere neither with monocyte count nor with the monocyte subpopulation partitioning. When excluding patients receiving GC, splenectomized patients had a higher monocyte count compared to non-splenectomized patients (1.0 vs 0.5G/L, p=0.008), with no difference in monocyte subset repartition.
Conclusion
Using multiparameter flow cytometry analysis, we demonstrated the expansion of iMo in untreated ITP patients. GC treatment led to the accumulation of cMo with reduced ncMo proportion, hence should be considered when interpreting the monocyte subset partitioning. These data suggest a potential role of monocytes in ITP pathogenesis and clinical response to GC therapy.
Disclosures
Mahevas:Sanofi: Research Funding; Novartis: Honoraria; Amgen: Honoraria. Michel:Sanofi: Consultancy; Alexion: Consultancy; Sobi: Consultancy; argenx: Honoraria; UCB: Honoraria; Novartis: Consultancy. Wagner-Ballon:Novartis: Honoraria; Alexion: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal